How the Integrated Behavioral Health Care enables a better patient experience and cost effectiveness for the Healthcare Delivery Organization
Digital Health is going to make medicine more personalized and efficient. Every area of the hospital will benefit from the use of technology if it adequately implemented into the clinical practice. This is probably the biggest hurdle most startups are struggling with.
Integrated Behavioral Health Care
Value-based healthcare is changing the way we think about healthcare innovation and the debate is not always about technology.
Cost savings community-based interventions can come from new approaches used by Healthcare Delivery Organizations (HDO). One of these is the Integrated Behavioral Health Care (IBHC), that can be described as:
The care that results from a practice team of primary care and behavioral health clinicians, working together with patients and families, using a systematic and cost-effective approach to provide patient-centered care for a defined population – Peak 2013.
The Dimock Center, a community health center based in Boston and serving more than 19,000 people annually, adopted this model.
The Integrated Behavioral Health Care represents a paradigm shift that requires a cultural transformation, with a shared vision, personal relationships across disciplines (e.g. primary care and psychology) and valuing the expertise of the team members. Particulars focus has to be given to the patient experience for what it concerns the location where the services are delivered. For example, the studio of the psychologist should be closed to the GP doctor.
Four pillars of the Behavioral Health Integration
- Improving patient experience (e.g. layout of the hospital)
- Improving population health. For example, prevention and early intervention with the Primary care Physician and Universal Behavioral Health Screening (e.g. Financial Problems)
- Reducing costs, for instance, reduction of Fee for service in the Accountable Care Organizations
- Provider satisfaction, for example, reducing burnout, “this latter is a public health crisis”
Source: TRIPLE (or Quadruple) AIM
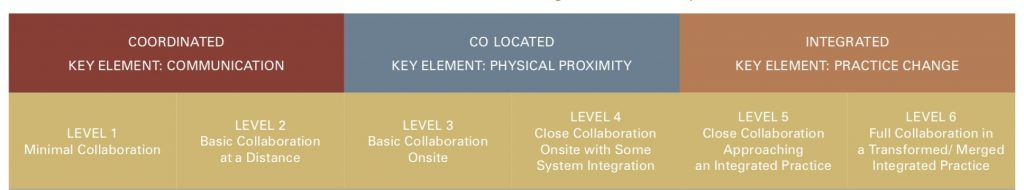
There are different types of Behavioral Health Integration. The Standard Framework for Levels of Integrated Care (SAHMSA-HRSA) is based on six levels divided into three main categories:
From Level 1, where collaboration between different specialties is minimal to Level 6, where there is a full collaboration, a unique culture, patients and providers view the service delivered as single health system treating the whole person.
The implementation of the Behavioral Health Model
The integration of services happens at all levels, including the top management, with unified leadership and administrative staff across the whole organization. This makes possible to save costs and avoid budget conflicts.
The implementation of the Behavioral Health Model can take years since it requires a relevant re-organization of the services. It is interesting to point out that it is a cultural change achievable without new technologies and involving the processes of the HDO.
BHM redefines primary care as a biopsychosocial model, considering the person as a whole, reducing stigma for behavioral health services, fostering new collaborations between healthcare professionals and saving costs for the healthcare delivery organizations (e.g. hospital).
The transformation towards the Behavioral Health Model can be leveraged by technology, data interoperability of EMR is key to support this process.